
Get more information on Pharmacy Benefit Management Market - Request Free Sample Report
The Pharmacy Benefit Management Market size was estimated at USD 553.4 billion in 2023 and is expected to reach USD 934.9 billion by 2032 at a CAGR of 6.0% during the forecast period of 2024-2032.
Pharmacy Benefit Management (PBM) Market: A Surge in Growth Driven by Innovation and Rising Healthcare Expenditures
Accelerating Market Expansion Fueled by Increased Demand for Cost-Effective Drug Management Solutions
The pharmacy benefit management (PBM) market is experiencing robust growth, driven by several critical factors such as the increasing adoption of PBM systems, rising healthcare expenditure, and a growing demand for prescription medications. As global health spending escalates, adopting advanced software solutions for managing drug inventories, enhancing accessibility, and reducing medication costs is expected to propel market expansion during the forecast period. For instance, Canada's healthcare expenditure surged to USD 344 billion in 2023 from USD 334 billion in 2022, as the Canadian Institute for Health Information reported. This increase in spending is anticipated to foster the integration of state-of-the-art PBM systems, making essential medications more affordable and accessible. The escalating reliance on pharmacy benefit management solutions further enhances operational accuracy, improves pharmacy safety, and boosts patient health outcomes. Noteworthy is Elixir, the PBM division of Rite Aid, which joined the Pharmaceutical Care Management Association (PCMA) in March 2022 to enhance patient access to cost-effective prescription drugs, contributing to market growth.
| Factor/Innovation | Description | Positive Impact on PBM Market |
|---|---|---|
| Increasing Healthcare Expenditure | Rising global spending on healthcare drives demand for efficient drug management solutions. | Expands market opportunities for PBM systems to optimize drug pricing and manage costs effectively. |
| Advanced PBM Software Solutions | Adoption of cutting-edge PBM software for managing drug inventories and reducing costs. | Enhances operational efficiency, improves accessibility to medications, and supports cost reduction. |
| Integration of Machine Learning (ML) | ML algorithms used for predictive analytics, fraud detection, and claim processing. | Improves accuracy, reduces claim processing times, and enhances cost savings. |
| Integration of Artificial Intelligence (AI) | AI-driven insights for personalized medication management and improved patient outcomes. | Streamlines operations, enhances patient care, and fosters innovation in drug management. |
| Partnerships and Mergers | Strategic alliances and acquisitions in the PBM sector to streamline services. | Enhances service delivery, optimizes drug pricing, and expands market reach. |
| Increased Adoption of Specialty Pharmacy Services | Growth in demand for specialty medications and handling services. | Drives demand for PBM services to manage high-cost specialty drugs effectively. |
| Government Regulations and Reimbursements | New regulatory guidelines and favorable reimbursement policies for PBMs. | Creates a supportive environment for market growth and enhances consumer protection. |
| Innovative Formulary Management | Introduction of cost-effective formulary recommendations and alternatives. | Promotes competition among drug manufacturers and reduces medication costs. |
| Growing Chronic Disease Prevalence | Rise in chronic diseases necessitating effective drug management solutions. | Increases demand for PBM services to handle complex medication regimens and cost management. |
Additionally, significant players in the PBM industry are actively developing innovative software and solutions, further driving market progress. For example, in July 2023, Prime Therapeutics introduced formulary recommendations to provide more cost-effective alternatives to Humira, fostering competition among drug manufacturers and reducing costs for patients. However, the market faces challenges such as resistance to adopting pharmacy automation systems and stringent regulatory processes related to confidentiality, which may impede growth.
Despite these obstacles, the market is projected to continue its upward trajectory, supported by innovations like the integration of machine learning (ML) and artificial intelligence (AI) into pharmacy workflows. These technologies streamline operations, reduce claim processing times, and help identify fraudulent claims, significantly enhancing efficiency and cost savings for PBM providers. Overall, the rising adoption of PBM services among insurers, pharmacies, and drug manufacturers, coupled with technological advancements, positions the market for substantial growth in the coming years.
| Company | Key Strategies & Innovations | Recent Developments |
|---|---|---|
| CVS Health | Expanding PBM services, strategic acquisitions | Recent acquisition/partnership news |
| Optum, Inc. | Advanced analytics, AI integration | New software solutions launched |
| Prime Therapeutics | Cost-effective formulary alternatives | Recent formulary updates |
| Elixir Rx Solutions | Enhancing patient access, new partnerships | Membership in PCMA |
| Anthem, Inc. | Integration with healthcare services | New collaboration announcements |
Market Dynamics: Drivers and Restraints
Drivers:
Rising Healthcare Expenditure and Pharmaceutical Costs
The growing global healthcare expenditure is a primary driver of the pharmacy benefit management (PBM) market's expansion. A critical factor fueling this growth is the escalating pharmaceutical costs, particularly due to the rising prevalence of chronic diseases worldwide. As the demand for effective treatment solutions increases, pharmaceutical companies are focusing on developing high-priced branded medications for chronic conditions, resulting in a significant rise in pharmaceutical spending. Additionally, the rising costs of medications and the increasing volume of prescriptions globally have heightened the healthcare burden. In response, there is a growing need for PBM services to manage drug prices and pharmaceutical spending more effectively. PBM services enable healthcare providers, insurers, and pharmacies to control costs while ensuring access to necessary treatments. Consequently, the adoption of PBM systems is expanding as they play a crucial role in optimizing drug pricing and utilization, making medications more affordable and accessible. This increasing need for cost containment and efficient management of pharmaceutical resources is expected to drive the PBM market's growth over the forecast period.
Restraints:
Lack of Transparency in Profit Revenues
The adoption of pharmacy benefit management (PBM) systems is hindered by a significant lack of transparency in profit revenues. Many stakeholders, including healthcare providers, insurers, and patients, express concern about the opaque nature of how PBM companies generate profits, particularly regarding drug pricing and rebates. This perceived lack of clarity creates distrust and slows down the widespread acceptance of PBM services. Without a clear understanding of revenue flow, stakeholders may be hesitant to fully integrate PBM solutions, thereby restraining market growth. Addressing this transparency issue is crucial for fostering broader adoption and enhancing market acceptance.
By Service
In 2023, the specialty pharmacy services segment held the highest market revenue at 49%. Specialty pharmacies are developed to efficiently supply medications with exceptional handling, stockpiling, and distribution requirements to address unusual or complicated medical conditions. The rising incidence of rare and chronic diseases is driving demand for specialty medications. High-priced pharmaceuticals need to be affordable for most patients, which boosts the demand for pharmacy benefit management services to make specialty medications more manageable in terms of cost. Consequently, specialty pharmacy services dominate the industry. Several market participants are engaged in strategic efforts to drive market growth, including the development of advanced solutions and partnerships to enhance service delivery.
By End User
In 2023, the healthcare providers segment led the pharmacy benefit management (PBM) market's growth, driven by a surge in mergers and acquisitions involving PBM services by insurance companies and healthcare providers. This trend highlights a strategic effort to streamline operations and enhance service offerings. For instance, the partnership between First Medical Health Plan Inc. and Abarca Health LLC established a three-year collaboration to deliver pharmacy benefit administration services. Such partnerships enable healthcare providers to integrate PBM services more efficiently, improving patient care and reducing prescription costs. Additionally, the increasing presence of health insurance companies in both developed and emerging markets is contributing to the expansion of PBM services. As healthcare systems evolve and the demand for affordable medications rises, insurance providers are investing in PBM systems to enhance their service portfolios. This collaboration between healthcare providers and insurance companies not only fosters market growth but also helps optimize drug pricing, improve access to necessary treatments, and enhance overall healthcare outcomes. These developments are expected to fuel the healthcare providers segment's dominance in the PBM market during the forecast period.
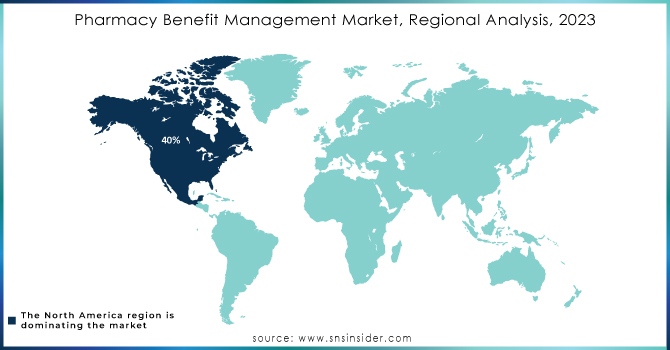
Regional Analysis
North America
North America dominated the pharmacy benefit management (PBM) market in 2023, holding a 40% share valued at USD 206.3 million. This dominance is primarily due to the concentration of major pharmaceutical manufacturers, insurance companies, PBM service providers, and retail pharmacy chains, many of which are based in the United States. The widespread adoption of health insurance among the U.S. population has further fueled market growth. Additionally, over 50% of the U.S. population suffers from chronic diseases, increasing the demand for PBM services. The market's expansion in North America is also supported by rising insurance policy adoption rates, high healthcare expenditures, and a growing number of health insurance providers. Favorable government reimbursement policies play a crucial role in driving market growth, as many U.S. patients rely on reimbursements for treatment.
Europe
Europe is experiencing the fastest compound annual growth rate (CAGR) during the forecast period. The region's growth is driven by a high percentage of patients covered by medical insurance, a favorable regulatory environment for PBMs, and the expanding presence of pharmacy benefit administrators. The UK holds the largest market share in the region, while France is witnessing the fastest growth, contributing to Europe's strengthening position in the global PBM market.
Need any customization research on Pharmacy Benefit Management Market - Enquiry Now
Key Players
CVS Health
SS&C Technologies, Inc.
Elixir Rx Solutions, LLC
Anthem, Inc.
Optum, Inc.
Centene Corporation
Abarca Health LLC
Medimpact
Cigna
Change Healthcare
CaptureRx Inc.
Benecard Services, LLC
Express Scripts Holding Company
McKesson Corporation
Sea Rainbow
Vidalink
Prime Therapeutics
Humana Pharmacy Solutions
Magellan Rx Management
MeridianRx
Recent Developments
February 2024: The New York State Department of Financial Services (DFS) superintendent introduced new regulatory guidelines for Pharmacy Benefit Managers (PBMs) aimed at enhancing consumer protections and addressing anti-competitive practices within the state.
February 2024: Better Therapeutics Inc. secured a rebate agreement with a leading Pharmacy Benefits Manager (PBM) in the U.S. This agreement focuses on the PBM’s commercial clients, allowing plan participants to incorporate AspyreRx into their formularies while qualifying for rebates.
| Report Attributes | Details |
| Market Size in 2023 | US$ 553.4 Billion |
| Market Size by 2032 | US$ 934.9 Billion |
| CAGR | CAGR of 6.0% From 2024 to 2032 |
| Base Year | 2023 |
| Forecast Period | 2024-2032 |
| Historical Data | 2020-2022 |
| Report Scope & Coverage | Market Size, Segments Analysis, Competitive Landscape, Regional Analysis, DROC & SWOT Analysis, Forecast Outlook |
| Key Segments | • By Service (Retail pharmacy services, Specialty pharmacy services, Benefit plan design & consultation, and Others) • By End User (Healthcare Providers and Employers) |
| Regional Analysis/Coverage | North America (US, Canada, Mexico), Europe (Eastern Europe [Poland, Romania, Hungary, Turkey, Rest of Eastern Europe] Western Europe] Germany, France, UK, Italy, Spain, Netherlands, Switzerland, Austria, Rest of Western Europe]), Asia Pacific (China, India, Japan, South Korea, Vietnam, Singapore, Australia, Rest of Asia Pacific), Middle East & Africa (Middle East [UAE, Egypt, Saudi Arabia, Qatar, Rest of Middle East], Africa [Nigeria, South Africa, Rest of Africa], Latin America (Brazil, Argentina, Colombia Rest of Latin America) |
| Company Profiles | CVS Health, SS&C Technologies, Inc., Elixir Rx Solutions, LLC, Anthem, Inc., Optum, Inc., Centene Corporation, Abarca Health LLC., Medimpact, Cigna, Change Healthcare, CaptureRx Inc., Benecard Services, LLC, Express Scripts Holding Company, McKesson Corporation, Sea Rainbow, Vidalink, Prime Therapeutics, Humana Pharmacy Solutions, Magellan Rx Management, MeridianRx and others. |
| Key Drivers | • Rising Healthcare Expenditure and Pharmaceutical Costs |
| Market Opportunity | • A lack of transparency in profit revenues is to blame for limiting adoption. |
Ans: The pharmacy benefit management market is anticipated to expand by 6.0% from 2024 to 2032.
Ans: The pharmacy benefit management market size was valued at USD 553.4 billion in 2023.
Ans: The pharmacy benefit management market size was expected to grow to USD 934.9 billion by 2032.
Ans: North America is dominating the pharmacy benefit management market.
Ans: Increasing pharmaceutical expenses drive market growth of pharmacy benefit management market.
1. Introduction
1.1 Market Definition
1.2 Scope (Inclusion and Exclusions)
1.3 Research Assumptions
2. Executive Summary
2.1 Market Overview
2.2 Regional Synopsis
2.3 Competitive Summary
3. Research Methodology
3.1 Top-Down Approach
3.2 Bottom-up Approach
3.3. Data Validation
3.4 Primary Interviews
4. Market Dynamics Impact Analysis
4.1 Market Driving Factors Analysis
4.1.2 Drivers
4.1.2 Restraints
4.1.3 Opportunities
4.1.4 Challenges
4.2 PESTLE Analysis
4.3 Porter’s Five Forces Model
5. Statistical Insights and Trends Reporting
5.1 Adoption Rates, 2023
5.2 User Demographics, By User Type and Roles, 2023
5.3 Feature Analysis, by Feature Type
5.4 Cost Analysis, by Software
5.6 Integration Capabilities
5.7 Regulatory Compliance, by Region
6. Competitive Landscape
6.1 List of Major Companies, By Region
6.2 Market Share Analysis, By Region
6.3 Service Benchmarking
6.3.1 Service specifications and features
6.3.2 Pricing
6.4 Strategic Initiatives
6.4.1 Marketing and promotional activities
6.4.2 Distribution and Supply Chain Strategies
6.4.3 Expansion plans and new Service launches
6.4.4 Strategic partnerships and collaborations
6.5 Technological Advancements
6.6 Market Positioning and Branding
7. Pharmacy Benefit Management Market Segmentation, by Service
7.1 Chapter Overview
7.2 Retail Pharmacy Services
7.2.1 Retail Pharmacy Services Market Trends Analysis (2020-2032)
7.2.2 Retail Pharmacy Services Market Size Estimates and Forecasts to 2032 (USD Million)
7.3 Specialty Pharmacy Services
7.3.1 Specialty Pharmacy Services Market Trends Analysis (2020-2032)
7.3.2 Specialty Pharmacy Services Market Size Estimates and Forecasts to 2032 (USD Million)
7.4 Benefit Plan Design & Consultation
7.4.1 Benefit Plan Design & Consultation Market Trends Analysis (2020-2032)
7.4.2 Benefit Plan Design & Consultation Market Size Estimates and Forecasts to 2032 (USD Million)
7.5 Others
7.5.1 Others Market Trends Analysis (2020-2032)
7.5.2 Others Market Size Estimates and Forecasts to 2032 (USD Million)
8. Pharmacy Benefit Management Market Segmentation, by End User
8.1 Chapter Overview
8.2 Healthcare Providers
8.2.1 Healthcare Providers Market Trends Analysis (2020-2032)
8.2.2 Healthcare Providers Market Size Estimates and Forecasts to 2032 (USD Million)
8.3 Employers
8.3.1 Employers Market Trends Analysis (2020-2032)
8.3.2 Employers Market Size Estimates and Forecasts to 2032 (USD Million)
9. Regional Analysis
9.1 Chapter Overview
9.2 North America
9.2.1 Trends Analysis
9.2.2 North America Pharmacy Benefit Management Market Estimates and Forecasts, by Country (2020-2032) (USD Million)
9.2.3 North America Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.2.4 North America Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.2.5 USA
9.2.5.1 USA Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.2.5.2 USA Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.2.6 Canada
9.2.6.1 Canada Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.2.6.2 Canada Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.2.7 Mexico
9.2.7.1 Mexico Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.2.7.2 Mexico Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.3 Europe
9.3.1 Eastern Europe
9.3.1.1 Trends Analysis
9.3.1.2 Eastern Europe Pharmacy Benefit Management Market Estimates and Forecasts, by Country (2020-2032) (USD Million)
9.3.1.3 Eastern Europe Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.3.1.4 Eastern Europe Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.3.1.5 Poland
9.3.1.5.1 Poland Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.3.1.5.2 Poland Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.3.1.6 Romania
9.3.1.6.1 Romania Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.3.1.6.2 Romania Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.3.1.7 Hungary
9.3.1.7.1 Hungary Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.3.1.7.2 Hungary Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.3.1.8 Turkey
9.3.1.8.1 Turkey Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.3.1.8.2 Turkey Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.3.1.9 Rest of Eastern Europe
9.3.1.9.1 Rest of Eastern Europe Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.3.1.9.2 Rest of Eastern Europe Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.3.2 Western Europe
9.3.2.1 Trends Analysis
9.3.2.2 Western Europe Pharmacy Benefit Management Market Estimates and Forecasts, by Country (2020-2032) (USD Million)
9.3.2.3 Western Europe Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.3.2.4 Western Europe Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.3.2.5 Germany
9.3.2.5.1 Germany Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.3.2.5.2 Germany Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.3.2.6 France
9.3.2.6.1 France Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.3.2.6.2 France Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.3.2.7 UK
9.3.2.7.1 UK Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.3.2.7.2 UK Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.3.2.8 Italy
9.3.2.8.1 Italy Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.3.2.8.2 Italy Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.3.2.9 Spain
9.3.2.9.1 Spain Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.3.2.9.2 Spain Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.3.2.10 Netherlands
9.3.2.10.1 Netherlands Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.3.2.10.2 Netherlands Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.3.2.11 Switzerland
9.3.2.11.1 Switzerland Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.3.2.11.2 Switzerland Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.3.2.12 Austria
9.3.2.12.1 Austria Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.3.2.12.2 Austria Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.3.2.13 Rest of Western Europe
9.3.2.13.1 Rest of Western Europe Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.3.2.13.2 Rest of Western Europe Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.4 Asia Pacific
9.4.1 Trends Analysis
9.4.2 Asia Pacific Pharmacy Benefit Management Market Estimates and Forecasts, by Country (2020-2032) (USD Million)
9.4.3 Asia Pacific Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.4.4 Asia Pacific Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.4.5 China
9.4.5.1 China Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.4.5.2 China Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.4.6 India
9.4.5.1 India Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.4.5.2 India Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.4.5 Japan
9.4.5.1 Japan Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.4.5.2 Japan Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.4.6 South Korea
9.4.6.1 South Korea Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.4.6.2 South Korea Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.4.7 Vietnam
9.4.7.1 Vietnam Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.2.7.2 Vietnam Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.4.8 Singapore
9.4.8.1 Singapore Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.4.8.2 Singapore Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.4.9 Australia
9.4.9.1 Australia Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.4.9.2 Australia Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.4.10 Rest of Asia Pacific
9.4.10.1 Rest of Asia Pacific Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.4.10.2 Rest of Asia Pacific Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.5 Middle East and Africa
9.5.1 Middle East
9.5.1.1 Trends Analysis
9.5.1.2 Middle East Pharmacy Benefit Management Market Estimates and Forecasts, by Country (2020-2032) (USD Million)
9.5.1.3 Middle East Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.5.1.4 Middle East Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.5.1.5 UAE
9.5.1.5.1 UAE Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.5.1.5.2 UAE Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.5.1.6 Egypt
9.5.1.6.1 Egypt Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.5.1.6.2 Egypt Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.5.1.7 Saudi Arabia
9.5.1.7.1 Saudi Arabia Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.5.1.7.2 Saudi Arabia Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.5.1.8 Qatar
9.5.1.8.1 Qatar Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.5.1.8.2 Qatar Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.5.1.9 Rest of Middle East
9.5.1.9.1 Rest of Middle East Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.5.1.9.2 Rest of Middle East Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.5.2 Africa
9.5.2.1 Trends Analysis
9.5.2.2 Africa Pharmacy Benefit Management Market Estimates and Forecasts, by Country (2020-2032) (USD Million)
9.5.2.3 Africa Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.5.2.4 Africa Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.5.2.5 South Africa
9.5.2.5.1 South Africa Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.5.2.5.2 South Africa Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.5.2.6 Nigeria
9.5.2.6.1 Nigeria Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.5.2.6.2 Nigeria Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.6 Latin America
9.6.1 Trends Analysis
9.6.2 Latin America Pharmacy Benefit Management Market Estimates and Forecasts, by Country (2020-2032) (USD Million)
9.6.3 Latin America Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.6.4 Latin America Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.6.5 Brazil
9.6.5.1 Brazil Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.6.5.2 Brazil Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.6.6 Argentina
9.6.6.1 Argentina Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.6.6.2 Argentina Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.6.7 Colombia
9.6.7.1 Colombia Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.6.7.2 Colombia Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
9.6.8 Rest of Latin America
9.6.8.1 Rest of Latin America Pharmacy Benefit Management Market Estimates and Forecasts, by Service (2020-2032) (USD Million)
9.6.8.2 Rest of Latin America Pharmacy Benefit Management Market Estimates and Forecasts, by End User (2020-2032) (USD Million)
10. Company Profiles
10.1 CVS Health
10.1.1 Company Overview
10.1.2 Financial
10.1.3 Services/ Services Offered
110.1.4 SWOT Analysis
10.2 SS&C Technologies, Inc.
10.2.1 Company Overview
10.2.2 Financial
10.2.3 Services/ Services Offered
10.2.4 SWOT Analysis
10.3 Elixir Rx Solutions, LLC
10.3.1 Company Overview
10.3.2 Financial
10.3.3 Services/ Services Offered
10.3.4 SWOT Analysis
10.4 Anthem, Inc.
10.4.1 Company Overview
10.4.2 Financial
10.4.3 Services/ Services Offered
10.4.4 SWOT Analysis
10.5 Optum, Inc.
10.5.1 Company Overview
10.5.2 Financial
10.5.3 Services/ Services Offered
10.5.4 SWOT Analysis
10.6 Centene Corporation
10.6.1 Company Overview
10.6.2 Financial
10.6.3 Services/ Services Offered
10.6.4 SWOT Analysis
10.7 Abarca Health LLC.
10.7.1 Company Overview
10.7.2 Financial
10.7.3 Services/ Services Offered
10.7.4 SWOT Analysis
10.8 Medimpact
10.8.1 Company Overview
10.8.2 Financial
10.8.3 Services/ Services Offered
10.8.4 SWOT Analysis
10.9 Cigna
10.9.1 Company Overview
10.9.2 Financial
10.9.3 Services/ Services Offered
10.9.4 SWOT Analysis
10.10 Change Healthcare
10.9.1 Company Overview
10.9.2 Financial
10.9.3 Services/ Services Offered
10.9.4 SWOT Analysis
11. Use Cases and Best Practices
12. Conclusion
An accurate research report requires proper strategizing as well as implementation. There are multiple factors involved in the completion of good and accurate research report and selecting the best methodology to compete the research is the toughest part. Since the research reports we provide play a crucial role in any company’s decision-making process, therefore we at SNS Insider always believe that we should choose the best method which gives us results closer to reality. This allows us to reach at a stage wherein we can provide our clients best and accurate investment to output ratio.
Each report that we prepare takes a timeframe of 350-400 business hours for production. Starting from the selection of titles through a couple of in-depth brain storming session to the final QC process before uploading our titles on our website we dedicate around 350 working hours. The titles are selected based on their current market cap and the foreseen CAGR and growth.
The 5 steps process:
Step 1: Secondary Research:
Secondary Research or Desk Research is as the name suggests is a research process wherein, we collect data through the readily available information. In this process we use various paid and unpaid databases which our team has access to and gather data through the same. This includes examining of listed companies’ annual reports, Journals, SEC filling etc. Apart from this our team has access to various associations across the globe across different industries. Lastly, we have exchange relationships with various university as well as individual libraries.

Step 2: Primary Research
When we talk about primary research, it is a type of study in which the researchers collect relevant data samples directly, rather than relying on previously collected data. This type of research is focused on gaining content specific facts that can be sued to solve specific problems. Since the collected data is fresh and first hand therefore it makes the study more accurate and genuine.
We at SNS Insider have divided Primary Research into 2 parts.
Part 1 wherein we interview the KOLs of major players as well as the upcoming ones across various geographic regions. This allows us to have their view over the market scenario and acts as an important tool to come closer to the accurate market numbers. As many as 45 paid and unpaid primary interviews are taken from both the demand and supply side of the industry to make sure we land at an accurate judgement and analysis of the market.
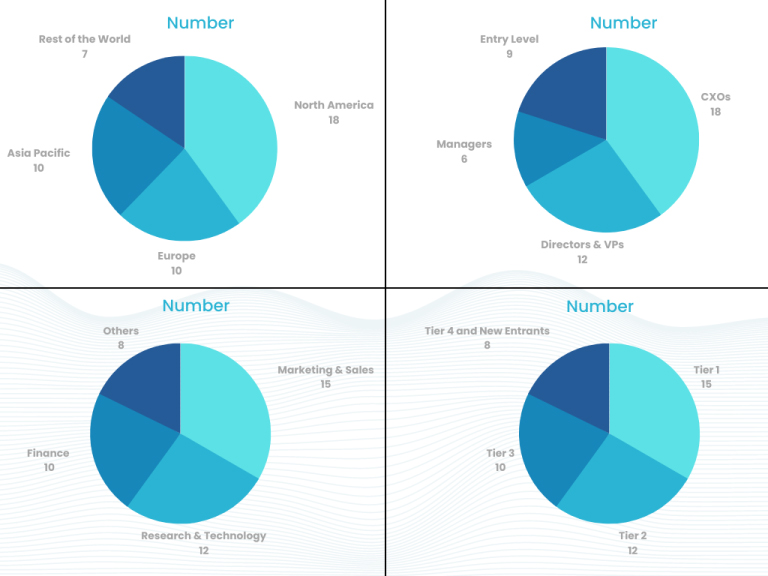
This step involves the triangulation of data wherein our team analyses the interview transcripts, online survey responses and observation of on filed participants. The below mentioned chart should give a better understanding of the part 1 of the primary interview.
Part 2: In this part of primary research the data collected via secondary research and the part 1 of the primary research is validated with the interviews from individual consultants and subject matter experts.
Consultants are those set of people who have at least 12 years of experience and expertise within the industry whereas Subject Matter Experts are those with at least 15 years of experience behind their back within the same space. The data with the help of two main processes i.e., FGDs (Focused Group Discussions) and IDs (Individual Discussions). This gives us a 3rd party nonbiased primary view of the market scenario making it a more dependable one while collation of the data pointers.
Step 3: Data Bank Validation
Once all the information is collected via primary and secondary sources, we run that information for data validation. At our intelligence centre our research heads track a lot of information related to the market which includes the quarterly reports, the daily stock prices, and other relevant information. Our data bank server gets updated every fortnight and that is how the information which we collected using our primary and secondary information is revalidated in real time.

Step 4: QA/QC Process
After all the data collection and validation our team does a final level of quality check and quality assurance to get rid of any unwanted or undesired mistakes. This might include but not limited to getting rid of the any typos, duplication of numbers or missing of any important information. The people involved in this process include technical content writers, research heads and graphics people. Once this process is completed the title gets uploader on our platform for our clients to read it.
Step 5: Final QC/QA Process:
This is the last process and comes when the client has ordered the study. In this process a final QA/QC is done before the study is emailed to the client. Since we believe in giving our clients a good experience of our research studies, therefore, to make sure that we do not lack at our end in any way humanly possible we do a final round of quality check and then dispatch the study to the client.
Key Segmentation
By Service
Retail pharmacy services
Specialty pharmacy services
Benefit plan design & consultation
Others
By End User
Healthcare Providers
Employers
Request for Segment Customization as per your Business Requirement: Segment Customization Request
Regional Coverage:
North America
US
Canada
Mexico
Europe
Eastern Europe
Poland
Romania
Hungary
Turkey
Rest of Eastern Europe
Western Europe
Germany
France
UK
Italy
Spain
Netherlands
Switzerland
Austria
Rest of Western Europe
Asia Pacific
China
India
Japan
South Korea
Vietnam
Singapore
Australia
Rest of Asia Pacific
Middle East & Africa
Middle East
UAE
Egypt
Saudi Arabia
Qatar
Rest of the Middle East
Africa
Nigeria
South Africa
Rest of Africa
Latin America
Brazil
Argentina
Colombia
Rest of Latin America
Request for Country Level Research Report: Country Level Customization Request
Available Customization
With the given market data, SNS Insider offers customization as per the company’s specific needs. The following customization options are available for the report:
Product Analysis
Criss-Cross segment analysis (e.g. Product X Application)
Product Matrix which gives a detailed comparison of the product portfolio of each company
Geographic Analysis
Additional countries in any of the regions
Company Information
Detailed analysis and profiling of additional market players (Up to five)
The IoT Medical Devices Market Size was valued at USD 41.4 billion in 2023 and is expected to reach USD 503.6 billion by 2032 and grow at a CAGR of 32.0% over the forecast period 2024-2032.
The Albumin Market Size was valued at USD 6.15 billion in 2023, and is expected to reach USD 10.5 billion by 2032, and grow at a CAGR of 6.1% over the forecast period 2024-2032.
Pet Services Market Size was valued at USD 3.64 Billion in 2023 and is expected to reach USD 6.95 billion by 2032, growing at a CAGR of 7.46% over the forecast period 2024-2032.
The Digital Twins in Healthcare Market size was valued at USD 1.41 billion in 2023, and is expected to reach USD 28.88 billion by 2032, and grow at a CAGR of 40.01% over the forecast period 2024-2032.
Pathology Laboratories Market was valued at USD 355.56 billion in 2023 and is expected to reach USD 720.60 billion by 2032, growing at a CAGR of 8.13% from 2024-2032.
The Sleep Disorder Treatment Market was valued at $20.3 billion in 2023 and is expected to reach $40.0 billion by 2032 at a CAGR of 7.84% from 2024 to 2032.
Hi! Click one of our member below to chat on Phone